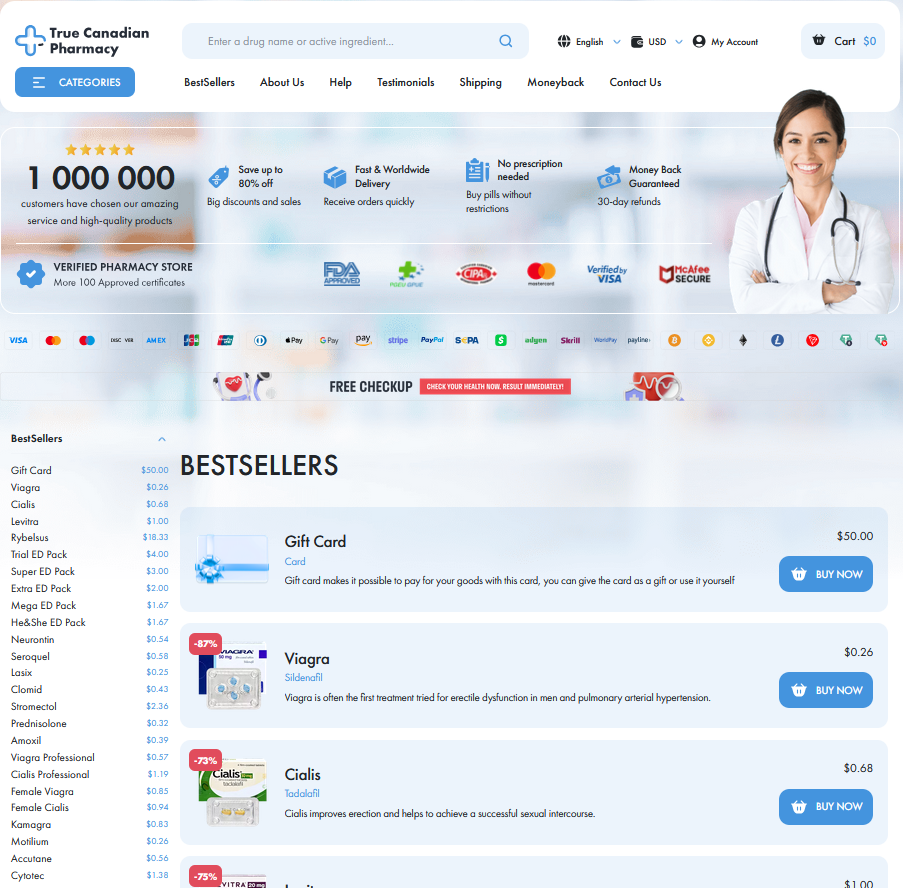
To Buy Isotretinoin Online Visit Our Pharmacy ↓
 Mental Health and Isotretinoin: Separating Myth from Evidence
Mental Health and Isotretinoin: Separating Myth from Evidence
Isotretinoin and Mood: Separating Fact from Fear
I used to read alarming headlines, then as a clinician I watched patients transform; balancing acne relief with concerns about mood is a real emotional storyline. Large studies show most people do not develop new depression during treatment, though rare cases and patient feelings deserve attentive listening. Science separates causation from coincidence: temporal links happen, but confounding factors like severe acne, sleep loss, and social distress often explain mood changes.
Clinicians should discuss risks openly, screen for prior mental health issues, and set a plan for check-ins. Patients should report mood shifts early; stopping or adjusting treatment can be effective. This balanced approach helps care teams Seperate fear from evidence while supporting both skin and psyche.
| Item | Note |
|---|---|
| Overall risk | Low for most people |
| Action | Screen, monitor, report promptly |
| Anecdotes | Use as signal not evidence |
| Call | if mood severely changes |
What Studies Really Say about Depression Risk

When clinicians and patients examine the literature on isotretinoin and mood, the narrative is more complex than headlines imply. Large cohorts and systematic reviews mostly find no consistent causal link between isotretinoin and depression, though isolated case reports and temporal associations keep concern alive. Confounding factors—severe acne itself, past psychiatric history, and life stressors—often muddy interpretation.
Clinicians should screen for prior mood disorders, discuss risks honestly, and monitor patients closely early in treatment when changes are likely. Most studies suggest benefits of acne improvement on quality of life often outweigh risks, but any new or worsening symptoms deserve prompt evaluation and reporting so interventions can occur; the approach is cautionary, evidence-based, and definately not alarmist.
Biological Mechanisms: How Retinoids Could Affect Brain
Researchers have explored how skin drugs can affect the brain. Isotretinoin crosses the blood–brain barrier and binds retinoid receptors that regulate genes linked to mood. Understanding pathways clarifies why some patients report mood shifts in certain circumstances.
Retinoid signalling influences neurogenesis, synaptic plasticity and neurotransmitters like serotonin. Animal and cellular studies show changes in BDNF and inflammation, whereas human findings are mixed.
Clinicians can use this biology to balance acne benefits against uncommon psychiatric risks and to inform consent. Ongoing research must Seperate causation from coincidence and improve screening strategies.
Patient Stories Versus Data: Interpreting Anecdotes Wisely

Personal stories about isotretinoin can be powerful: a friend's sudden sadness or a blog's dramatic recovery shapes perception. Yet anecdotes reflect single paths, not averages. Clinicians weigh these narratives alongside controlled studies to avoid Teh bias of assuming causation from coincidence and to inform safer care.
Patients should share concerns openly; clinicians should contextualize reports with evidence, screening for prior mood disorders and life stresses. This balanced approach helps detect true signals among noise, supports informed consent, fosters trust, and guides intervention when needed, reducing harm while respecting individual experiance
Risk Factors and Screening before Starting Isotretinoin
I often meet patients who worry about mood changes when offered isotretinoin; clear screening calms fear and builds trust.
Baseline assessment should note past depression, substance use, sleep, and social supports; a brief questionnaire can Seperate high and low risk.
Blood tests and contraceptive counseling matter for physical safety, while collaborative care plans link patients to mental health resources quickly.
Clinicians should schedule follow ups, educate families, and encourage immediate reporting of mood shifts; early action reduces harm and preserves acne treatment benefits.
| Factor | Action |
|---|---|
| History | Refer immediately |
| Sleep | Monitor |
Practical Guidance: Monitoring, Reporting, and Mental Health
Starting isotretinoin should feel like a partnership: clinicians explain baseline screening, mood history, and clear expectations, while patients report changes promptly. Brief standardized check-ins every 4–8 weeks let teams catch early warning signs and offer support or dose adjustments. This approach keeps care patient-centered and reduces anxiety about rare events that occassionally arise.
If mood shifts occur, contact your provider immediately; 24/7 help lines and emergency services exist for suicidal thoughts. Documenting symptoms, dates, and medicines helps clinicians weigh risks and benefits. Most people do well but a low threshold for mental health referral is wise. Keep family involved when possible for extra oversight. Learn more from authoritative sources: FDA: Isotretinoin MedlinePlus: Isotretinoin
